Interpreting Medical Terminology: Gastroenterology
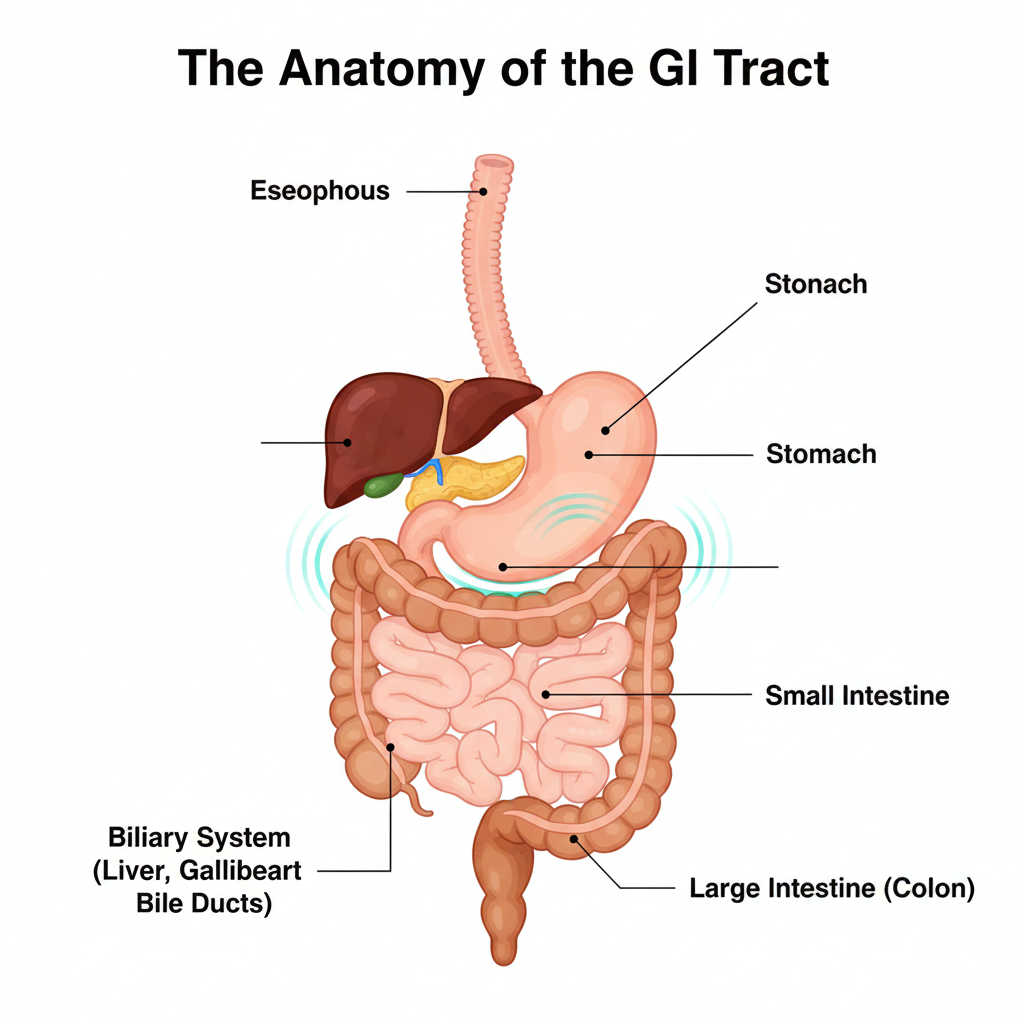
The digestive system, or gastrointestinal (GI) tract, is a complex series of organs and pathways responsible for processing nutrients and managing waste. In gastroenterology, symptoms such as “abdominal pain” or “indigestion” are often overlapping and non-specific. For a medical interpreter, providing a precise and faithful rendering of both the clinician’s terminology and the patient’s experiential descriptions is essential for accurate diagnosis and effective treatment planning.
Precision in Gastrointestinal Interpretation
Patients frequently describe GI symptoms using everyday sensory or experiential language. Interpreters must convey these descriptions accurately to allow clinicians to evaluate the mechanical or functional nature of the issue without any distortion of meaning.
- Patient: “It feels like a fire in my chest after I eat.” Interpreter: “The patient reports a burning sensation in the chest following meals.”
- Patient: “Food keeps getting stuck in my throat.” Interpreter: “The patient reports a sensation of food being lodged in the throat.”
- Why this matters: General terms such as “stomach ache” can refer to a wide range of conditions. Accurately conveying a patient’s exact description helps a clinician determine if the symptom is consistent with GERD (acid reflux) or Dysphagia (difficulty swallowing).
Distinguishing Between Similar Conditions
Gastroenterology includes many conditions and procedures that sound similar but indicate very different clinical paths. Incomplete or generalized interpretation can compromise patient understanding and lead to treatment approaches that are not indicated.
- IBD vs. IBS:
- IBD (Inflammatory Bowel Disease): Includes conditions like Crohn’s Disease and Ulcerative Colitis, which involve chronic inflammation and visible damage to the digestive tract.
- IBS (Irritable Bowel Syndrome): A functional disorder that causes pain and discomfort but does not cause inflammation or permanent damage to the organs.
- Endoscopy vs. Colonoscopy: While both involve using a camera (endoscope) to view the digestive tract, an Endoscopy (EGD) looks at the upper GI tract (esophagus, stomach, and duodenum), while a Colonoscopy examines the large intestine (colon).
Clinical Significance of Patient Descriptions
Accurately rendering how a patient describes their symptoms—without interpretation or substitution—is critical in gastrointestinal care.
- Melena: A patient might report “black, sticky stools.” This should be rendered exactly as stated. If an interpreter substitutes this with “dark stools,” the clinician might miss a critical sign of upper GI bleeding.
- Hematochezia: A patient might report “bright red blood when I go to the bathroom.” This specific detail points to lower GI bleeding, whereas a generalized term like “bleeding” is less diagnostically useful.
GI Systems and Procedure Classification
Gastroenterological evaluation focuses on the function of the digestive organs and the movement of food and waste through the body. Clinicians assess how signals, enzymes, and muscles work together within the GI tract.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): A specialized procedure used to study the bile ducts, pancreatic duct, and gallbladder.
- Ascites: The accumulation of fluid in the abdomen, often associated with advanced liver disease. If an interpreter omits clinical qualifiers or simplifies the patient’s description of “swelling,” the clinician’s assessment of the severity of liver dysfunction may be affected.
Faithfully rendering the specific terminology used by clinicians and accurately conveying the patient’s description of events supports clinical evaluation. Generalizing or simplifying terminology may obscure distinctions that are relevant to diagnosis and life-saving treatment planning.



Leave Your Comments Below