Precision in Neurological Interpretation
Patients often describe neurological symptoms using everyday sensory language. In neurological encounters, interpreters must convey these descriptions accurately and completely so clinicians can evaluate nervous system function without loss or distortion of meaning.
General terms such as “dizziness” may refer to a range of sensations with different clinical implications. Accurately conveying the patient’s exact description allows the clinician to determine whether the symptom may be consistent with vertigo or another condition.
Neurology also includes conditions that resemble neurological disorders but have different underlying causes.
- PNES (Psychogenic Non-Epileptic Seizures): Events that resemble epileptic seizures but are not associated with abnormal electrical activity in the brain.
If qualifiers such as “psychogenic” or “non-epileptic” are omitted, clinical decision-making may be affected, potentially leading to treatment approaches that are not indicated and may expose the patient to unnecessary risk.
Interpreters must also accurately render commonly used neurological abbreviations and terminology, including:
- TIA (Transient Ischemic Attack): A temporary neurological event that resolves but indicates increased risk of stroke.
- CVA (Cerebrovascular Accident): The medical term for a stroke.
- LP (Lumbar Puncture): A procedure used to collect cerebrospinal fluid for diagnostic evaluation.
- MS (Multiple Sclerosis): A chronic disease affecting the central nervous system.
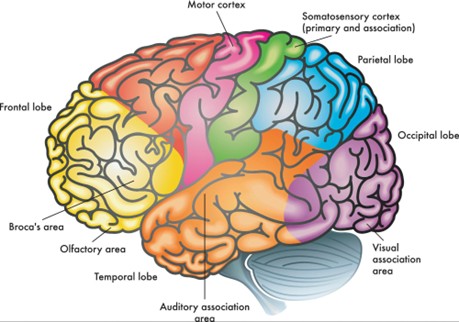
The nervous system regulates essential functions including movement, sensation, speech, and consciousness. In neurological encounters, incomplete or generalized interpretation can compromise patient understanding and clinical assessment.
When clinicians discuss conditions such as a subdural hematoma versus an epidural hematoma, the interpreter must ensure the information is conveyed fully and accurately, without additions, omissions, or substitutions. Precision is critical in neurological care.
Distinguishing between aphasia and dysarthria is particularly important in stroke-related encounters. Although both may be described as “difficulty speaking,” they reflect different neurological mechanisms.
- Aphasia: A disorder of language processing that may affect the ability to find, understand, or produce words, despite intact speech muscles.
- Dysarthria: A motor speech disorder in which weakness or incoordination of the muscles used for speech affects clarity and articulation, while language formulation may remain intact.
If a patient states, “I can’t say the words,” and this is rendered as “the patient’s speech is slurred,” critical information about the nature of the speech difficulty may be altered. This can influence how the clinician evaluates the symptom, potentially shifting attention from a language-processing impairment to a motor speech issue.
Accurately conveying how the patient describes their speech difficulty—without interpretation or substitution—is essential in stroke care.
Neurological evaluation focuses on the function of the nervous system rather than isolated organs. Clinicians assess how signals are generated, transmitted, and processed within the central nervous system (CNS) and peripheral nervous system (PNS).
When a neurologist questions a patient, the goal is to determine whether symptoms may involve central or peripheral nervous system pathways. The interpreter’s role is to accurately and completely render both the patient’s descriptions and the clinician’s questions to support this assessment.
Broad terms may be insufficient in neurological contexts. For example, the term “seizure” encompasses multiple event types with distinct clinical implications, treatment approaches, and potential outcomes.
- Generalized tonic-clonic seizure: A seizure involving both hemispheres of the brain, typically associated with loss of consciousness and bilateral motor activity.
- Focal onset seizure: A seizure that begins in a specific area of the brain and may occur with preserved or altered awareness.
Faithfully rendering the specific terminology used by clinicians and accurately conveying the patient’s description of events supports clinical evaluation. Generalizing, substituting, or simplifying terminology may obscure distinctions that are relevant to diagnosis and treatment planning.



Leave Your Comments Below