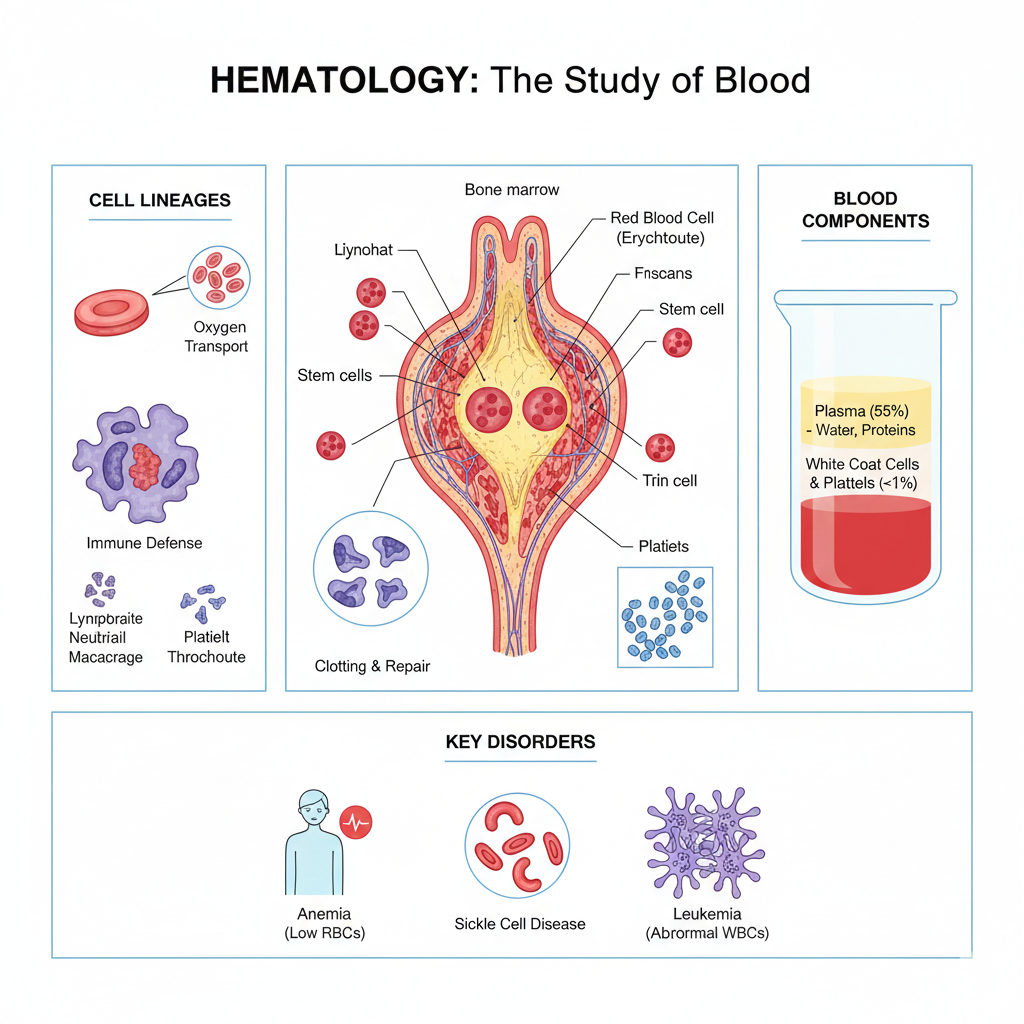
Blood is a dynamic fluid that serves as the body’s primary transport system, delivering oxygen, nutrients, and immune cells to every organ. In hematology, the branch of medicine focused on blood and blood-forming tissues, the terminology used to describe cellular counts and chemical balances shapes the entire course of clinical care. An experienced interpreter understands these precise distinctions and communicates them accurately, supporting a clear understanding for both the patient and the physician to ensure appropriate treatment decisions.
Patients often describe symptoms of blood disorders using non-medical, experiential language. When interpreters render these descriptions into clinically relevant terminology, they must do so carefully and accurately, ensuring that the patient’s meaning is preserved without adding, omitting, or altering clinical content.
- Anemia: A patient may say, “I feel like I have no energy and my heart is racing.” An interpreter can accurately report this as the patient experiencing fatigue and palpitations, allowing the physician to determine if these are signs of a low red blood cell count.
- Thrombocytopenia: A patient might report “strange tiny red dots on my skin” or “bruising for no reason.” An interpreter can convey this as the patient noticing petechiae or unexplained ecchymosis, leaving the clinical assessment of a low platelet count to the physician.
- Why this matters: Generalizing a patient’s description of “tiredness” might cause a clinician to overlook the specific physical markers of a hematological condition. Faithfully conveying the patient’s exact words allows the physician to assess the clinical significance themselves.
Hematology contains terms that may sound similar or involve complex acronyms that have very different meanings. Dropping a prefix or misinterpreting an abbreviation can change the understanding of whether a condition is a benign deficiency or a malignant process.
- CBC (Complete Blood Count): A standard test used to evaluate overall health and detect a wide range of disorders, including anemia, infection, and leukemia.
- Hgb vs. Hct: While both relate to red blood cells, Hemoglobin (Hgb) measures the oxygen-carrying protein, while Hematocrit (Hct) measures the percentage of total blood volume made up of red cells.
- Leukemia vs. Lymphoma:
- Leukemia: A type of cancer that typically starts in the bone marrow and results in high numbers of abnormal white blood cells.
- Lymphoma: A cancer that begins in the cells of the lymph system, which is part of the immune system.
- Interpreter considerations: When clinicians discuss specific conditions such as hemophilia versus von Willebrand disease, the interpreter must ensure the information is conveyed fully and accurately, without additions or substitutions, as the clotting factors involved are distinct and require different treatments.
Hematological evaluation focuses on the function and production of blood cells rather than a single isolated organ. Clinicians assess how cells are generated in the bone marrow and how they function within the circulatory system.
- Bone Marrow Aspiration: A procedure used to collect a sample of the liquid portion of the bone marrow for diagnostic evaluation.
- Coagulation: The process by which blood changes from a liquid to a gel, forming a blood clot.
- Sickle Cell Disease: A group of inherited red blood cell disorders where the cells become hard and sticky and shaped like a C-shaped farm tool.
Providing only a partial summary or “the gist” of a hematology consult can risk serious miscommunication. By accurately conveying distinctions such as neutropenia (low white blood cell count) versus pancytopenia (a reduction in all types of blood cells), interpreters ensure patients receive the full information needed to understand their condition, while leaving clinical judgment to the physician. Precision is critical in hematological care.



Leave Your Comments Below